- Research article
- Open access
- Published: 04 February 2020

Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health
- Xinguang Chen 1 ,
- Xiangfan Chen 2 &
- Hong Yan 2
BMC Public Health volume 20 , Article number: 156 ( 2020 ) Cite this article
112k Accesses
82 Citations
81 Altmetric
Metrics details
Marijuana is the most commonly used illicit drug in the United States. More and more states legalized medical and recreational marijuana use. Adolescents and emerging adults are at high risk for marijuana use. This ecological study aims to examine historical trends in marijuana use among youth along with marijuana legalization.
Data ( n = 749,152) were from the 31-wave National Survey on Drug Use and Health (NSDUH), 1979–2016. Current marijuana use, if use marijuana in the past 30 days, was used as outcome variable. Age was measured as the chronological age self-reported by the participants, period was the year when the survey was conducted, and cohort was estimated as period subtracted age. Rate of current marijuana use was decomposed into independent age, period and cohort effects using the hierarchical age-period-cohort (HAPC) model.
After controlling for age, cohort and other covariates, the estimated period effect indicated declines in marijuana use in 1979–1992 and 2001–2006, and increases in 1992–2001 and 2006–2016. The period effect was positively and significantly associated with the proportion of people covered by Medical Marijuana Laws (MML) (correlation coefficients: 0.89 for total sample, 0.81 for males and 0.93 for females, all three p values < 0.01), but was not significantly associated with the Recreational Marijuana Laws (RML). The estimated cohort effect showed a historical decline in marijuana use in those who were born in 1954–1972, a sudden increase in 1972–1984, followed by a decline in 1984–2003.
The model derived trends in marijuana use were coincident with the laws and regulations on marijuana and other drugs in the United States since the 1950s. With more states legalizing marijuana use in the United States, emphasizing responsible use would be essential to protect youth from using marijuana.
Peer Review reports
Introduction
Marijuana use and laws in the united states.
Marijuana is one of the most commonly used drugs in the United States (US) [ 1 ]. In 2015, 8.3% of the US population aged 12 years and older used marijuana in the past month; 16.4% of adolescents aged 12–17 years used in lifetime and 7.0% used in the past month [ 2 ]. The effects of marijuana on a person’s health are mixed. Despite potential benefits (e.g., relieve pain) [ 3 ], using marijuana is associated with a number of adverse effects, particularly among adolescents. Typical adverse effects include impaired short-term memory, cognitive impairment, diminished life satisfaction, and increased risk of using other substances [ 4 ].
Since 1937 when the Marijuana Tax Act was issued, a series of federal laws have been subsequently enacted to regulate marijuana use, including the Boggs Act (1952), Narcotics Control Act (1956), Controlled Substance Act (1970), and Anti-Drug Abuse Act (1986) [ 5 , 6 ]. These laws regulated the sale, possession, use, and cultivation of marijuana [ 6 ]. For example, the Boggs Act increased the punishment of marijuana possession, and the Controlled Substance Act categorized the marijuana into the Schedule I Drugs which have a high potential for abuse, no medical use, and not safe to use without medical supervision [ 5 , 6 ]. These federal laws may have contributed to changes in the historical trend of marijuana use among youth.
Movements to decriminalize and legalize marijuana use
Starting in the late 1960s, marijuana decriminalization became a movement, advocating reformation of federal laws regulating marijuana [ 7 ]. As a result, 11 US states had taken measures to decriminalize marijuana use by reducing the penalty of possession of small amount of marijuana [ 7 ].
The legalization of marijuana started in 1993 when Surgeon General Elder proposed to study marijuana legalization [ 8 ]. California was the first state that passed Medical Marijuana Laws (MML) in 1996 [ 9 ]. After California, more and more states established laws permitting marijuana use for medical and/or recreational purposes. To date, 33 states and the District of Columbia have established MML, including 11 states with recreational marijuana laws (RML) [ 9 ]. Compared with the legalization of marijuana use in the European countries which were more divided that many of them have medical marijuana registered as a treatment option with few having legalized recreational use [ 10 , 11 , 12 , 13 ], the legalization of marijuana in the US were more mixed with 11 states legalized medical and recreational use consecutively, such as California, Nevada, Washington, etc. These state laws may alter people’s attitudes and behaviors, finally may lead to the increased risk of marijuana use, particularly among young people [ 13 ]. Reported studies indicate that state marijuana laws were associated with increases in acceptance of and accessibility to marijuana, declines in perceived harm, and formation of new norms supporting marijuana use [ 14 ].
Marijuana harm to adolescents and young adults
Adolescents and young adults constitute a large proportion of the US population. Data from the US Census Bureau indicate that approximately 60 million of the US population are in the 12–25 years age range [ 15 ]. These people are vulnerable to drugs, including marijuana [ 16 ]. Marijuana is more prevalent among people in this age range than in other ages [ 17 ]. One well-known factor for explaining the marijuana use among people in this age range is the theory of imbalanced cognitive and physical development [ 4 ]. The delayed brain development of youth reduces their capability to cognitively process social, emotional and incentive events against risk behaviors, such as marijuana use [ 18 ]. Understanding the impact of marijuana laws on marijuana use among this population with a historical perspective is of great legal, social and public health significance.
Inconsistent results regarding the impact of marijuana laws on marijuana use
A number of studies have examined the impact of marijuana laws on marijuana use across the world, but reported inconsistent results [ 13 ]. Some studies reported no association between marijuana laws and marijuana use [ 14 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ], some reported a protective effect of the laws against marijuana use [ 24 , 26 ], some reported mixed effects [ 27 , 28 ], while some others reported a risk effect that marijuana laws increased marijuana use [ 29 , 30 ]. Despite much information, our review of these reported studies revealed several limitations. First of all, these studies often targeted a short time span, ignoring the long period trend before marijuana legalization. Despite the fact that marijuana laws enact in a specific year, the process of legalization often lasts for several years. Individuals may have already changed their attitudes and behaviors before the year when the law is enacted. Therefore, it may not be valid when comparing marijuana use before and after the year at a single time point when the law is enacted and ignoring the secular historical trend [ 19 , 30 , 31 ]. Second, many studies adapted the difference-in-difference analytical approach designated for analyzing randomized controlled trials. No US state is randomized to legalize the marijuana laws, and no state can be established as controls. Thus, the impact of laws cannot be efficiently detected using this approach. Third, since marijuana legalization is a public process, and the information of marijuana legalization in one state can be easily spread to states without the marijuana laws. The information diffusion cannot be ruled out, reducing the validity of the non-marijuana law states as the controls to compare the between-state differences [ 31 ].
Alternatively, evidence derived based on a historical perspective may provide new information regarding the impact of laws and regulations on marijuana use, including state marijuana laws in the past two decades. Marijuana users may stop using to comply with the laws/regulations, while non-marijuana users may start to use if marijuana is legal. Data from several studies with national data since 1996 demonstrate that attitudes, beliefs, perceptions, and use of marijuana among people in the US were associated with state marijuana laws [ 29 , 32 ].
Age-period-cohort modeling: looking into the past with recent data
To investigate historical trends over a long period, including the time period with no data, we can use the classic age-period-cohort modeling (APC) approach. The APC model can successfully discompose the rate or prevalence of marijuana use into independent age, period and cohort effects [ 33 , 34 ]. Age effect refers to the risk associated with the aging process, including the biological and social accumulation process. Period effect is risk associated with the external environmental events in specific years that exert effect on all age groups, representing the unbiased historical trend of marijuana use which controlling for the influences from age and birth cohort. Cohort effect refers to the risk associated with the specific year of birth. A typical example is that people born in 2011 in Fukushima, Japan may have greater risk of cancer due to the nuclear disaster [ 35 ], so a person aged 80 in 2091 contains the information of cancer risk in 2011 when he/she was born. Similarly, a participant aged 25 in 1979 contains information on the risk of marijuana use 25 years ago in 1954 when that person was born. With this method, we can describe historical trends of marijuana use using information stored by participants in older ages [ 33 ]. The estimated period and cohort effects can be used to present the unbiased historical trend of specific topics, including marijuana use [ 34 , 36 , 37 , 38 ]. Furthermore, the newly established hierarchical APC (HAPC) modeling is capable of analyzing individual-level data to provide more precise measures of historical trends [ 33 ]. The HAPC model has been used in various fields, including social and behavioral science, and public health [ 39 , 40 ].
Several studies have investigated marijuana use with APC modeling method [ 17 , 41 , 42 ]. However, these studies covered only a small portion of the decades with state marijuana legalization [ 17 , 42 ]. For example, the study conducted by Miech and colleagues only covered periods from 1985 to 2009 [ 17 ]. Among these studies, one focused on a longer state marijuana legalization period, but did not provide detailed information regarding the impact of marijuana laws because the survey was every 5 years and researchers used a large 5-year age group which leads to a wide 10-year birth cohort. The averaging of the cohort effects in 10 years could reduce the capability of detecting sensitive changes of marijuana use corresponding to the historical events [ 41 ].
Purpose of the study
In this study, we examined the historical trends in marijuana use among youth using HAPC modeling to obtain the period and cohort effects. These two effects provide unbiased and independent information to characterize historical trends in marijuana use after controlling for age and other covariates. We conceptually linked the model-derived time trends to both federal and state laws/regulations regarding marijuana and other drug use in 1954–2016. The ultimate goal is to provide evidence informing federal and state legislation and public health decision-making to promote responsible marijuana use and to protect young people from marijuana use-related adverse consequences.
Materials and methods
Data sources and study population.
Data were derived from 31 waves of National Survey on Drug Use and Health (NSDUH), 1979–2016. NSDUH is a multi-year cross-sectional survey program sponsored by the Substance Abuse and Mental Health Services Administration. The survey was conducted every 3 years before 1990, and annually thereafter. The aim is to provide data on the use of tobacco, alcohol, illicit drug and mental health among the US population.
Survey participants were noninstitutionalized US civilians 12 years of age and older. Participants were recruited by NSDUH using a multi-stage clustered random sampling method. Several changes were made to the NSDUH after its establishment [ 43 ]. First, the name of the survey was changed from the National Household Survey on Drug Abuse (NHSDA) to NSDUH in 2002. Second, starting in 2002, adolescent participants receive $30 as incentives to improve the response rate. Third, survey mode was changed from personal interviews with self-enumerated answer sheets (before 1999) to the computer-assisted person interviews (CAPI) and audio computer-assisted self-interviews (ACASI) (since 1999). These changes may confound the historical trends [ 43 ], thus we used two dummy variables as covariates, one for the survey mode change in 1999 and another for the survey method change in 2002 to control for potential confounding effect.
Data acquisition
Data were downloaded from the designated website ( https://nsduhweb.rti.org/respweb/homepage.cfm ). A database was used to store and merge the data by year for analysis. Among all participants, data for those aged 12–25 years ( n = 749,152) were included. We excluded participants aged 26 and older because the public data did not provide information on single or two-year age that was needed for HAPC modeling (details see statistical analysis section). We obtained approval from the Institutional Review Board at the University of Florida to conduct this study.
Variables and measurements
Current marijuana use: the dependent variable. Participants were defined as current marijuana users if they reported marijuana use within the past 30 days. We used the variable harmonization method to create a comparable measure across 31-wave NSDUH data [ 44 ]. Slightly different questions were used in NSDUH. In 1979–1993, participants were asked: “When was the most recent time that you used marijuana or hash?” Starting in 1994, the question was changed to “How long has it been since you last used marijuana or hashish?” To harmonize the marijuana use variable, participants were coded as current marijuana users if their response to the question indicated the last time to use marijuana was within past 30 days.
Chronological age, time period and birth cohort were the predictors. (1) Chronological age in years was measured with participants’ age at the survey. APC modeling requires the same age measure for all participants [ 33 ]. Since no data by single-year age were available for participants older than 21, we grouped all participants into two-year age groups. A total of 7 age groups, 12–13, ..., 24–25 were used. (2) Time period was measured with the year when the survey was conducted, including 1979, 1982, 1985, 1988, 1990, 1991... 2016. (3). Birth cohort was the year of birth, and it was measured by subtracting age from the survey year.
The proportion of people covered by MML: This variable was created by dividing the population in all states with MML over the total US population. The proportion was computed by year from 1996 when California first passed the MML to 2016 when a total of 29 states legalized medical marijuana use. The estimated proportion ranged from 12% in 1996 to 61% in 2016. The proportion of people covered by RML: This variable was derived by dividing the population in all states with RML with the total US population. The estimated proportion ranged from 4% in 2012 to 21% in 2016. These two variables were used to quantitatively assess the relationships between marijuana laws and changes in the risk of marijuana use.
Covariates: Demographic variables gender (male/female) and race/ethnicity (White, Black, Hispanic and others) were used to describe the study sample.
Statistical analysis
We estimated the prevalence of current marijuana use by year using the survey estimation method, considering the complex multi-stage cluster random sampling design and unequal probability. A prevalence rate is not a simple indicator, but consisting of the impact of chronological age, time period and birth cohort, named as age, period and cohort effects, respectively. Thus, it is biased if a prevalence rate is directly used to depict the historical trend. HAPC modeling is an epidemiological method capable of decomposing prevalence rate into mutually independent age, period and cohort effects with individual-level data, while the estimated period and cohort effects provide an unbiased measure of historical trend controlling for the effects of age and other covariates. In this study, we analyzed the data using the two-level HAPC cross-classified random-effects model (CCREM) [ 36 ]:
Where M ijk represents the rate of marijuana use for participants in age group i (12–13, 14,15...), period j (1979, 1982,...) and birth cohort k (1954–55, 1956–57...); parameter α i (age effect) was modeled as the fixed effect; and parameters β j (period effect) and γ k (cohort effect) were modeled as random effects; and β m was used to control m covariates, including the two dummy variables assessing changes made to the NSDUH in 1999 and 2002, respectively.
The HAPC modeling analysis was executed using the PROC GLIMMIX. Sample weights were included to obtain results representing the total US population aged 12–25. A ridge-stabilized Newton-Raphson algorithm was used for parameter estimation. Modeling analysis was conducted for the overall sample, stratified by gender. The estimated age effect α i , period β j and cohort γ k (i.e., the log-linear regression coefficients) were directly plotted to visualize the pattern of change.
To gain insight into the relationship between legal events and regulations at the national level, we listed these events/regulations along with the estimated time trends in the risk of marijuana from HAPC modeling. To provide a quantitative measure, we associated the estimated period effect with the proportions of US population living with MML and RML using Pearson correlation. All statistical analyses for this study were conducted using the software SAS, version 9.4 (SAS Institute Inc., Cary, NC).
Sample characteristics
Data for a total of 749,152 participants (12–25 years old) from all 31-wave NSDUH covering a 38-year period were analyzed. Among the total sample (Table 1 ), 48.96% were male and 58.78% were White, 14.84% Black, and 18.40% Hispanic.
Prevalence rate of current marijuana use
As shown in Fig. 1 , the estimated prevalence rates of current marijuana use from 1979 to 2016 show a “V” shaped pattern. The rate was 27.57% in 1979, it declined to 8.02% in 1992, followed by a gradual increase to 14.70% by 2016. The pattern was the same for both male and female with males more likely to use than females during the whole period.
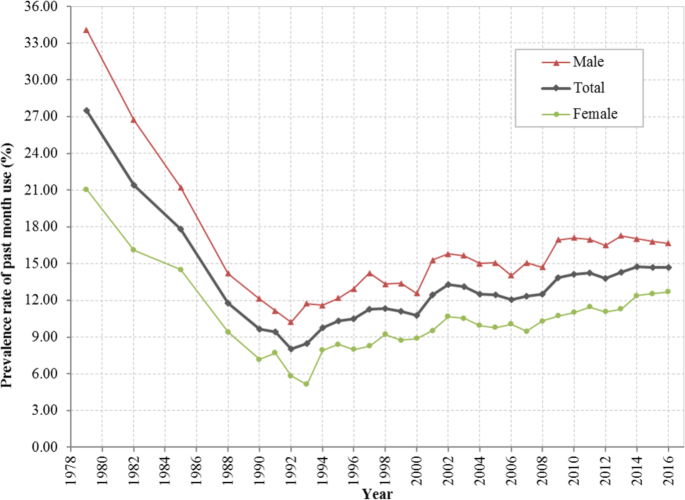
Prevalence rate (%) of current marijuana use among US residents 12 to 25 years of age during 1979–2016, overall and stratified by gender. Derived from data from the 1979–2016 National Survey on Drug Use and Health (NSDUH)
HAPC modeling and results
Estimated age effects α i from the CCREM [ 1 ] for current marijuana use are presented in Fig. 2 . The risk by age shows a 2-phase pattern –a rapid increase phase from ages 12 to 19, followed by a gradually declining phase. The pattern was persistent for the overall sample and for both male and female subsamples.
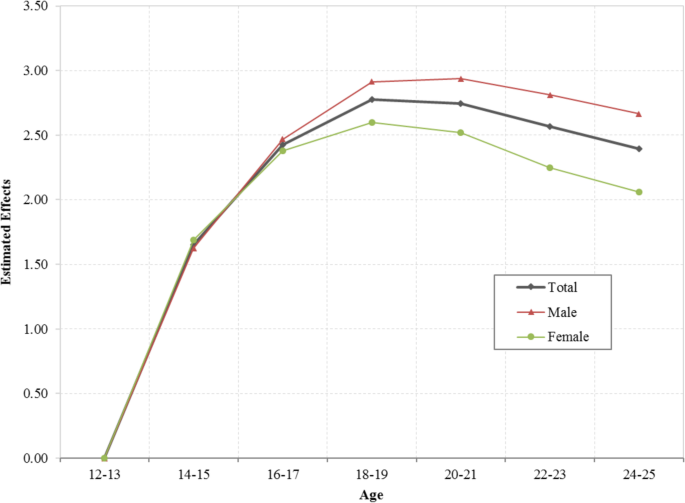
Age effect for the risk of current marijuana use, overall and stratified by male and female, estimated with hierarchical age-period-cohort modeling method with 31 waves of NSDUH data during 1979–2016. Age effect α i were log-linear regression coefficients estimated using CCREM (1), see text for more details
The estimated period effects β j from the CCREM [ 1 ] are presented in Fig. 3 . The period effect reflects the risk of current marijuana use due to significant events occurring over the period, particularly federal and state laws and regulations. After controlling for the impacts of age, cohort and other covariates, the estimated period effect indicates that the risk of current marijuana use had two declining trends (1979–1992 and 2001–2006), and two increasing trends (1992–2001 and 2006–2016). Epidemiologically, the time trends characterized by the estimated period effects in Fig. 3 are more valid than the prevalence rates presented in Fig. 1 because the former was adjusted for confounders while the later was not.
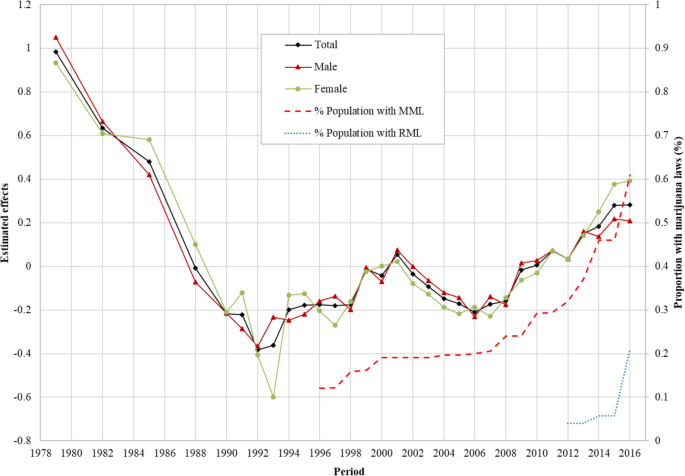
Period effect for the risk of marijuana use for US adolescents and young adults, overall and by male/female estimated with hierarchical age-period-cohort modeling method and its correlation with the proportion of US population covered by Medical Marijuana Laws and Recreational Marijuana Laws. Period effect β j were log-linear regression coefficients estimated using CCREM (1), see text for more details
Correlation of the period effect with proportions of the population covered by marijuana laws: The Pearson correlation coefficient of the period effect with the proportions of US population covered by MML during 1996–2016 was 0.89 for the total sample, 0.81 for male and 0.93 for female, respectively ( p < 0.01 for all). The correlation between period effect and proportion of US population covered by RML was 0.64 for the total sample, 0.59 for male and 0.49 for female ( p > 0.05 for all).
Likewise, the estimated cohort effects γ k from the CCREM [ 1 ] are presented in Fig. 4 . The cohort effect reflects changes in the risk of current marijuana use over the period indicated by the year of birth of the survey participants after the impacts of age, period and other covariates are adjusted. Results in the figure show three distinctive cohorts with different risk patterns of current marijuana use during 1954–2003: (1) the Historical Declining Cohort (HDC): those born in 1954–1972, and characterized by a gradual and linear declining trend with some fluctuations; (2) the Sudden Increase Cohort (SIC): those born from 1972 to 1984, characterized with a rapid almost linear increasing trend; and (3) the Contemporary Declining Cohort (CDC): those born during 1984 and 2003, and characterized with a progressive declining over time. The detailed results of HAPC modeling analysis were also shown in Additional file 1 : Table S1.

Cohort effect for the risk of marijuana use among US adolescents and young adults born during 1954–2003, overall and by male/female, estimated with hierarchical age-period-cohort modeling method. Cohort effect γ k were log-linear regression coefficients estimated using CCREM (1), see text for more details
This study provides new data regarding the risk of marijuana use in youth in the US during 1954–2016. This is a period in the US history with substantial increases and declines in drug use, including marijuana; accompanied with many ups and downs in legal actions against drug use since the 1970s and progressive marijuana legalization at the state level from the later 1990s till today (see Additional file 1 : Table S2). Findings of the study indicate four-phase period effect and three-phase cohort effect, corresponding to various historical events of marijuana laws, regulations and social movements.
Coincident relationship between the period effect and legal drug control
The period effect derived from the HAPC model provides a net effect of the impact of time on marijuana use after the impact of age and birth cohort were adjusted. Findings in this study indicate that there was a progressive decline in the period effect during 1979 and 1992. This trend was corresponding to a period with the strongest legal actions at the national level, the War on Drugs by President Nixon (1969–1974) President Reagan (1981–1989) [ 45 ], and President Bush (1989) [ 45 ],and the Anti-Drug Abuse Act (1986) [ 5 ].
The estimated period effect shows an increasing trend in 1992–2001. During this period, President Clinton advocated for the use of treatment to replace incarceration (1992) [ 45 ], Surgeon General Elders proposed to study marijuana legalization (1993–1994) [ 8 ], President Clinton’s position of the need to re-examine the entire policy against people who use drugs, and decriminalization of marijuana (2000) [ 45 ] and the passage of MML in eight US states.
The estimated period effect shows a declining trend in 2001–2006. Important laws/regulations include the Student Drug Testing Program promoted by President Bush, and the broadened the public schools’ authority to test illegal drugs among students given by the US Supreme Court (2002) [ 46 ].
The estimated period effect increases in 2006–2016. This is the period when the proportion of the population covered by MML progressively increased. This relation was further proved by a positive correlation between the estimated period effect and the proportion of the population covered by MML. In addition, several other events occurred. For example, over 500 economists wrote an open letter to President Bush, Congress and Governors of the US and called for marijuana legalization (2005) [ 47 ], and President Obama ended the federal interference with the state MML, treated marijuana as public health issues, and avoided using the term of “War on Drugs” [ 45 ]. The study also indicates that the proportion of population covered by RML was positively associated with the period effect although not significant which may be due to the limited number of data points of RML. Future studies may follow up to investigate the relationship between RML and rate of marijuana use.
Coincident relationship between the cohort effect and legal drug control
Cohort effect is the risk of marijuana use associated with the specific year of birth. People born in different years are exposed to different laws, regulations in the past, therefore, the risk of marijuana use for people may differ when they enter adolescence and adulthood. Findings in this study indicate three distinctive cohorts: HDC (1954–1972), SIC (1972–1984) and CDC (1984–2003). During HDC, the overall level of marijuana use was declining. Various laws/regulations of drug use in general and marijuana in particular may explain the declining trend. First, multiple laws passed to regulate the marijuana and other substance use before and during this period remained in effect, for example, the Marijuana Tax Act (1937), the Boggs Act (1952), the Narcotics Control Act (1956) and the Controlled Substance Act (1970). Secondly, the formation of government departments focusing on drug use prevention and control may contribute to the cohort effect, such as the Bureau of Narcotics and Dangerous Drugs (1968) [ 48 ]. People born during this period may be exposed to the macro environment with laws and regulations against marijuana, thus, they may be less likely to use marijuana.
Compared to people born before 1972, the cohort effect for participants born during 1972 and 1984 was in coincidence with the increased risk of using marijuana shown as SIC. This trend was accompanied by the state and federal movements for marijuana use, which may alter the social environment and public attitudes and beliefs from prohibitive to acceptive. For example, seven states passed laws to decriminalize the marijuana use and reduced the penalty for personal possession of small amount of marijuana in 1976 [ 7 ]. Four more states joined the movement in two subsequent years [ 7 ]. People born during this period may have experienced tolerated environment of marijuana, and they may become more acceptable of marijuana use, increasing their likelihood of using marijuana.
A declining cohort CDC appeared immediately after 1984 and extended to 2003. This declining cohort effect was corresponding to a number of laws, regulations and movements prohibiting drug use. Typical examples included the War on Drugs initiated by President Nixon (1980s), the expansion of the drug war by President Reagan (1980s), the highly-publicized anti-drug campaign “Just Say No” by First Lady Nancy Reagan (early 1980s) [ 45 ], and the Zero Tolerance Policies in mid-to-late 1980s [ 45 ], the Anti-Drug Abuse Act (1986) [ 5 ], the nationally televised speech of War on Drugs declared by President Bush in 1989 and the escalated War on Drugs by President Clinton (1993–2001) [ 45 ]. Meanwhile many activities of the federal government and social groups may also influence the social environment of using marijuana. For example, the Federal government opposed to legalize the cultivation of industrial hemp, and Federal agents shut down marijuana sales club in San Francisco in 1998 [ 48 ]. Individuals born in these years grew up in an environment against marijuana use which may decrease their likelihood of using marijuana when they enter adolescence and young adulthood.
This study applied the age-period-cohort model to investigate the independent age, period and cohort effects, and indicated that the model derived trends in marijuana use among adolescents and young adults were coincident with the laws and regulations on marijuana use in the United States since the 1950s. With more states legalizing marijuana use in the United States, emphasizing responsible use would be essential to protect youth from using marijuana.
Limitations
This study has limitations. First, study data were collected through a household survey, which is subject to underreporting. Second, no causal relationship can be warranted using cross-sectional data, and further studies are needed to verify the association between the specific laws/regulation and the risk of marijuana use. Third, data were available to measure single-year age up to age 21 and two-year age group up to 25, preventing researchers from examining the risk of marijuana use for participants in other ages. Lastly, data derived from NSDUH were nation-wide, and future studies are needed to analyze state-level data and investigate the between-state differences. Although a systematic review of all laws and regulations related to marijuana and other drugs is beyond the scope of this study, findings from our study provide new data from a historical perspective much needed for the current trend in marijuana legalization across the nation to get the benefit from marijuana while to protect vulnerable children and youth in the US. It provides an opportunity for stack-holders to make public decisions by reviewing the findings of this analysis together with the laws and regulations at the federal and state levels over a long period since the 1950s.
Availability of data and materials
The data of the study are available from the designated repository ( https://nsduhweb.rti.org/respweb/homepage.cfm ).
Abbreviations
Audio computer-assisted self-interviews
Age-period-cohort modeling
Computer-assisted person interviews
Cross-classified random-effects model
Contemporary Declining Cohort
Hierarchical age-period-cohort
Historical Declining Cohort
Medical Marijuana Laws
National Household Survey on Drug Abuse
National Survey on Drug Use and Health
Recreational Marijuana Laws
Sudden Increase Cohort
The United States
CDC. Marijuana and Public Health. 2017. Available from: https://www.cdc.gov/marijuana/index.htm . Accessed 13 June 2018.
SAMHSA. Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. 2016 [cited 2018 Jan 31]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm
Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda, Board on Population Health and Public Health Practice, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, D.C.: National Academies Press; 2017.
Collins C. Adverse health effects of marijuana use. N Engl J Med. 2014;371(9):879.
PubMed Google Scholar
Belenko SR. Drugs and drug policy in America: a documentary history. Westport: Greenwood Press; 2000.
Google Scholar
Gerber RJ. Legalizing marijuana: Drug policy reform and prohibition politics. Westport: Praeger; 2004.
Single EW. The impact of marijuana decriminalization: an update. J Public Health Policy. 1989:456–66.
Article CAS Google Scholar
SFChronicle. Ex-surgeon general backed legalizing marijuana before it was cool [Internet]. 2016 [cited 2018 Oct 7]. Available from: https://www.sfchronicle.com/business/article/Ex-surgeon-general-backed-legalizing-marijuana-6799348.php
PROCON. 31 Legal Medical Marijuana States and DC. 2018 [cited 2018 Oct 4]. Available from: https://medicalmarijuana.procon.org/view.resource.php?resourceID=000881
Bifulco M, Pisanti S. Medicinal use of cannabis in Europe: the fact that more countries legalize the medicinal use of cannabis should not become an argument for unfettered and uncontrolled use. EMBO Rep. 2015;16(2):130–2.
European Monitoring Centre for Drugs and Drug Addiction. Models for the legal supply of cannabis: recent developments (Perspectives on drugs). 2016. Available from: http://www.emcdda.europa.eu/publications/pods/legal-supply-of-cannabis . Accessed 10 Jan 2020.
European Monitoring Centre for Drugs and Drug Addiction. Cannabis policy: status and recent developments. 2017. Available from: http://www.emcdda.europa.eu/topics/cannabis-policy_en#section2 . Accessed 10 Jan 2020.
Hughes B, Matias J, Griffiths P. Inconsistencies in the assumptions linking punitive sanctions and use of cannabis and new psychoactive substances in Europe. Addiction. 2018;113(12):2155–7.
Article Google Scholar
Anderson DM, Hansen B, Rees DI. Medical marijuana laws and teen marijuana use. Am Law Econ Rev. 2015;17(2):495-28.
United States Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States, States, and Puerto Rico Commonwealth: April 1, 2010 to July 1, 2016 2016 Population Estimates. 2017 [cited 2018 Mar 14]. Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
Chen X, Yu B, Lasopa S, Cottler LB. Current patterns of marijuana use initiation by age among US adolescents and emerging adults: implications for intervention. Am J Drug Alcohol Abuse. 2017;43(3):261–70.
Miech R, Koester S. Trends in U.S., past-year marijuana use from 1985 to 2009: an age-period-cohort analysis. Drug Alcohol Depend. 2012;124(3):259–67.
Steinberg L. The influence of neuroscience on US supreme court decisions about adolescents’ criminal culpability. Nat Rev Neurosci. 2013;14(7):513–8.
Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, et al. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction. 2018;113(6):1003–16.
Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601–8.
Pacula RL, Chriqui JF, King J. Marijuana decriminalization: what does it mean in the United States? National Bureau of Economic Research; 2003.
Donnelly N, Hall W, Christie P. The effects of the Cannabis expiation notice system on the prevalence of cannabis use in South Australia: evidence from the National Drug Strategy Household Surveys 1985-95. Drug Alcohol Rev. 2000;19(3):265–9.
Gorman DM, Huber JC. Do medical cannabis laws encourage cannabis use? Int J Drug Policy. 2007;18(3):160–7.
Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013 Aug;103(8):1500–6.
Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana and alcohol use: the devil is in the details. National Bureau of Economic Research; 2013.
Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–12.
Stolzenberg L, D’Alessio SJ, Dariano D. The effect of medical cannabis laws on juvenile cannabis use. Int J Drug Policy. 2016;27:82–8.
Wang GS, Roosevelt G, Heard K. Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatr. 2013;167(7):630–3.
Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–6.
Chen X, Yu B, Stanton B, Cook RL, Chen D-GD, Okafor C. Medical marijuana laws and marijuana use among U.S. adolescents: evidence from michigan youth risk behavior surveillance data. J Drug Educ. 2018;47237918803361.
Chen X. Information diffusion in the evaluation of medical marijuana laws’ impact on risk perception and use. Am J Public Health. 2016;106(12):e8.
Chen X, Yu B, Stanton B, Cook RL, Chen DG, Okafor C. Medical marijuana laws and marijuana use among US adolescents: Evidence from Michigan youth risk behavior surveillance data. J Drug Educ. 2018;48(1-2):18-35.
Yang Y, Land K. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. Boca Raton: Chapman and Hall/CRC; 2013.
Yu B, Chen X. Age and birth cohort-adjusted rates of suicide mortality among US male and female youths aged 10 to 19 years from 1999 to 2017. JAMA Netw Open. 2019;2(9):e1911383.
Akiba S. Epidemiological studies of Fukushima residents exposed to ionising radiation from the Fukushima Daiichi nuclear power plant prefecture--a preliminary review of current plans. J Radiol Prot. 2012;32(1):1–10.
Yang Y, Land KC. Age-period-cohort analysis of repeated cross-section surveys: fixed or random effects? Sociol Methods Res. 2008;36(3):297–326.
O’Brien R. Age-period-cohort models: approaches and analyses with aggregate data. Boca Raton: Chapman and Hall/CRC; 2014.
Book Google Scholar
Chen X, Sun Y, Li Z, Yu B, Gao G, Wang P. Historical trends in suicide risk for the residents of mainland China: APC modeling of the archived national suicide mortality rates during 1987-2012. Soc Psychiatry Psychiatr Epidemiol. 2018;54(1):99–110.
Yang Y. Social inequalities in happiness in the United States, 1972 to 2004: an age-period-cohort analysis. Am Sociol Rev. 2008;73(2):204–26.
Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69(10):1439–48.
Kerr WC, Lui C, Ye Y. Trends and age, period and cohort effects for marijuana use prevalence in the 1984-2015 US National Alcohol Surveys. Addiction. 2018;113(3):473–81.
Johnson RA, Gerstein DR. Age, period, and cohort effects in marijuana and alcohol incidence: United States females and males, 1961-1990. Substance Use Misuse. 2000;35(6–8):925–48.
Substance Abuse and Mental Health Services Administration. Results from the 2013 NSDUH: Summary of National Findings, SAMHSA, CBHSQ. 2014 [cited 2018 Sep 23]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.htm
Bauer DJ, Hussong AM. Psychometric approaches for developing commensurate measures across independent studies: traditional and new models. Psychol Methods. 2009;14(2):101–25.
Drug Policy Alliance. A Brief History of the Drug War. 2018 [cited 2018 Sep 27]. Available from: http://www.drugpolicy.org/issues/brief-history-drug-war
NIDA. Drug testing in schools. 2017 [cited 2018 Sep 27]. Available from: https://www.drugabuse.gov/related-topics/drug-testing/faq-drug-testing-in-schools
Wikipedia contributors. Legal history of cannabis in the United States. 2015. Available from: https://en.wikipedia.org/w/index.php?title=Legal_history_of_cannabis_in_the_United_States&oldid=674767854 . Accessed 24 Oct 2017.
NORML. Marijuana law reform timeline. 2015. Available from: http://norml.org/shop/item/marijuana-law-reform-timeline . Accessed 24 Oct 2017.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Epidemiology, University of Florida, Gainesville, FL, 32608, USA
Bin Yu & Xinguang Chen
Department of Epidemiology and Health Statistics School of Health Sciences, Wuhan University, Wuhan, 430071, China
Xiangfan Chen & Hong Yan
You can also search for this author in PubMed Google Scholar
Contributions
BY designed the study, collected the data, conducted the data analysis, drafted and reviewed the manuscript; XGC designed the study and reviewed the manuscript. XFC and HY reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Hong Yan .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Institutional Review Board at the University of Florida. Data in the study were public available.
Consent for publication
All authors consented for the publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: table s1..
Estimated Age, Period, Cohort Effects for the Trend of Marijuana Use in Past Month among Adolescents and Emerging Adults Aged 12 to 25 Years, NSDUH, 1979-2016. Table S2. Laws at the federal and state levels related to marijuana use.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Yu, B., Chen, X., Chen, X. et al. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health. BMC Public Health 20 , 156 (2020). https://doi.org/10.1186/s12889-020-8253-4
Download citation
Received : 15 June 2019
Accepted : 21 January 2020
Published : 04 February 2020
DOI : https://doi.org/10.1186/s12889-020-8253-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents and young adults
- United States
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Journal of Cannabis Research
Aims and scope.
The Journal of Cannabis Research is an international, fully open access, peer-reviewed journal covering all topics pertaining to cannabis , including original research, perspectives, commentaries and protocols. Our goal is to provide an accessible outlet for expert interdisciplinary discourse on cannabis research.

Review of the current ongoing clinical trials exploring the possible anti-anxiety effects of cannabidiol
Authors: Rhenu Bhuller, Walter K. Schlage and Julia Hoeng
Association between cannabis use and physical activity in the United States based on legalization and health status
Authors: Ray M. Merrill, Kendyll Ashton-Hwang and Liliana Gallegos
Cannabis-related information sources among US residents: A probability-weighted nationally representative survey
Authors: Kevin F. Boehnke, Tristin Smith, Michael R. Elliott, Adrianne R. Wilson-Poe and Daniel J. Kruger
Attitudes toward driving after cannabis use: a systematic review
Authors: Bianca Boicu, Durr Al-Hakim, Yue Yuan and Jeffrey Brubacher
Changes in health-related quality of life over the first three months of medical marijuana use
Authors: Michelle R. Lent, Thomas R. McCalmont, Megan M. Short and Karen L. Dugosh
Most recent articles RSS
View all articles
Processing and extraction methods of medicinal cannabis: a narrative review
Authors: Masoumeh Pourseyed Lazarjani, Owen Young, Lidya Kebede and Ali Seyfoddin
Delta-8-THC: Delta-9-THC’s nicer younger sibling?
Authors: Jessica S. Kruger and Daniel J. Kruger
Cannabis consumption is associated with lower COVID-19 severity among hospitalized patients: a retrospective cohort analysis
Authors: Carolyn M. Shover, Peter Yan, Nicholas J. Jackson, Russell G. Buhr, Jennifer A. Fulcher, Donald P. Tashkin and Igor Barjaktarevic
Δ9-Tetrahydrocannabivarin (THCV): a commentary on potential therapeutic benefit for the management of obesity and diabetes
Authors: Amos Abioye, Oladapo Ayodele, Aleksandra Marinkovic, Risha Patidar, Adeola Akinwekomi and Adekunle Sanyaolu
Total and differential white blood cell count in cannabis users: results from the cross-sectional National Health and Nutrition Examination Survey, 2005–2016
Authors: Omayma Alshaarawy
Most accessed articles RSS
We are recruiting!
Journal of Cannabis Research is recruiting Associate Editors. As the growth of the journal continues, we are looking to expand our editorial team. If you have experience in any form of cannabis research, we would like to hear from you. Please follow the link below to find out more about the role and apply.
Webinar Series: Institute of Cannabis Research
Register for the Webinar Series hosted by the Institute of Cannabis Research and watch a comprehensive archive of cutting edge science presented by experts across the spectrum of cannabis research. The Cannabis Research Series hosted in collaboration with the Lambert Center at Thomas Jefferson University Cannabis Plant Science and Cultivation , hosted in collaboration with the Volcani Institute in Israel.
The Two Sides of Hemp
About the Institute
The Journal of Cannabis Research is the official publication of the Institute of Cannabis Research (ICR), which was established in June 2016 through an innovative partnership between Colorado State University Pueblo, the state of Colorado, and Pueblo County.
The ICR is the first US multi-disciplinary cannabis research center at a regional, comprehensive institution. The primary goal of the ICR is to conduct or fund research related to cannabis and publicly disseminate the results of the research, which it does so in partnership with the Journal. It also advises other Colorado-based higher education institutions on the development of a cannabis-related curriculum and supports the translation of discoveries into innovative applications that improve lives.
Find out more about the the Institute via the link below, as well as the Colorado state University–Pueblo website and Institute's research funding outcomes .

Affiliated with

An official publication of the Institute of Cannabis Research
- Editorial Board
- Instructions for Authors
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
Citation Impact 2023 Journal Impact Factor: 4.1 5-year Journal Impact Factor: 3.8 Source Normalized Impact per Paper (SNIP): 0.894 SCImago Journal Rank (SJR): 0.692
Speed 2023 Submission to first editorial decision (median days): 22 Submission to acceptance (median days): 211
Usage 2023 Downloads: 596,678 Altmetric mentions: 1,834
- More about our metrics
ISSN: 2522-5782
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Cannabis Unveiled: An Exploration of Marijuana’s History, Active Compounds, Effects, Benefits, and Risks on Human Health
Khaled m hasan.
- Author information
- Article notes
- Copyright and License information
Khaled M Hasan, Physician Assistant Department, School of Pharmacy and Health Professions, University of Maryland Eastern Shore, Hazel Hall, Suite 1042, Princess Anne, MD 21853, USA. Email: [email protected]
Received 2023 Mar 16; Accepted 2023 May 30; Collection date 2023.
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 License ( https://creativecommons.org/licenses/by-nc/4.0/ ) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages ( https://us.sagepub.com/en-us/nam/open-access-at-sage ).
Marijuana, also known as cannabis, is a psychoactive drug that comes from the Cannabis plant. Marijuana can be smoked, vaporized, or consumed through edibles in a variety of ways. Perception changes, changes in mood, and problems with coordination are all possible side effects. Marijuana is used for both recreational and medical purposes to treat a variety of health conditions. The literature review on the effects of marijuana on the human body has increased in recent years as more states legalize its use. It is important to investigate the benefits and harmful effects of marijuana on individuals due to the widespread use of cannabis-derived substances like marijuana for medical, recreational, and combined purposes. The paper will review different aspects of marijuana in 4 main domains. A thorough discussion of marijuana’s definition, history, mechanism of action, pharmacokinetics, and effects on human cells will be given in the first domain. The second domain will concentrate on marijuana’s negative effects, while the third domain will look at marijuana’s possible positive impacts, such as its usage in controlling multiple sclerosis, treating obesity, lowering social anxiety, and managing pain. The fourth domain will concentrate on marijuana’s effects on anxiety, educational attainment, and social consequences. Additionally, this paper also will provide a highlight of the history of marijuana use and governmental legislation, both of which play a significant role in determining how the public views marijuana. In conclusion, this paper provides a comprehensive review of marijuana’s effects, which may be of interest to a large readership. This review adds to the continuing discussion about the use of marijuana by analyzing the data that is currently available about the possible advantages and disadvantages of marijuana usage.
Keywords: Marijuana, cannabis, benefits, harmful, human body, social impacts, education attainment, legislation
Introduction
Marijuana and cannabis are often used interchangeably, but they technically refer to different things. “Cannabis” is the scientific name for the plant species that includes both marijuana and hemp. “Marijuana” specifically refers to the strains of cannabis that contain high levels of the psychoactive compound delta-9-tetrahydrocannabinol (THC), which is responsible for the plant’s intoxicating effects. “Hemp” on the other hand is a strain of cannabis that contains very low levels of THC and is mostly used for industrial and medical purposes. 1
The use of marijuana for both recreational and medicinal purposes can be traced back 6000 years. 1 THC interacts with cannabidiol (CB) receptors present in various organs, including the heart, brain, peripheral nervous system, skeletal muscles, and myocytes. 2 Marijuana is a naturally occurring substance that contains various chemicals. It is derived from hemp, a plant mainly grown for fiber production, and is part of the Cannabis species that contains cannabinoids. 3 The World Health Organization reports that marijuana is the most commonly used drug worldwide, with a global prevalence of 2.5%. It is a popular drug that can be consumed through smoking or orally. Marijuana usage is notably prevalent in the United States, with more than 22 million individuals aged 12 years or above having used it at least once in their lives. 4
The purpose of this review article is to provide an overview of marijuana, differentiate between the terms, highlight their historical use and touch upon the historical use of marijuana and governmental legislation. It also aims to establish the presence of various active substances in marijuana, explain their mechanism of action, and discuss the pharmacokinetics of cannabis. Furthermore, this article intends to explore the effects of marijuana on human cells, both beneficial and harmful, as well as its impact on education attainment, cardiovascular disorders, addiction potential, mental health, and its relationship with cancer. Lastly, it aims to address the social impacts of marijuana.
The history of marijuana
In the United States, marijuana was commonly consumed for recreational purposes until 1941, and it was also medically prescribed to alleviate symptoms such as arthritis, nausea, and labor pains. 1 , 3 During the 1930s, marijuana was portrayed as a substance that induced violent behavior in people, while in the 1960s it became a symbol of counterculture and rebellion against societal norms. 1 In 1970, the Controlled Substance Act classified marijuana as a Schedule 1 drug. 3 Despite this, the use of marijuana for both recreational and medicinal purposes has risen in the United States. This is in part due to a survey showing that 81% of American adults believe it has at least 1 medical benefit. 5
For more than 4000 years, marijuana has been utilized both for medicinal and recreational objectives. Its earliest known medicinal usage was documented in a Chinese artifact from 2700 B.C., which suggests that cannabis was used to treat a range of conditions including malaria, poor memory, gout, and rheumatism. 1 After originating in China, marijuana spread to other regions including Korea, India, and East Africa. The cultivation of hemp, which has strong fibers, also contributed to its spread. 1 , 2 For example, the Spanish brought it to America in the mid-1500s for cultivation. 1
The history of marijuana use and governmental legislation
In the United States, cannabis legalization has been a contentious issue in recent years. Cannabis has been legalized for medical and/or recreational use in some states, but not in others. As of April 2021, 36 states and the District of Columbia had legalized medical cannabis, while 15 states and the District of Columbia had legalized recreational cannabis, as reported by the Congressional Research Service. 6
The legalization of cannabis has been significantly influenced by public opinion. A 2021 Seat Exploration Center overview saw that 91% of Americans support the utilization of clinical pot, while 60% help the sanctioning of sporting marijuana. 7
The potential for tax revenue is yet another factor that is driving the legalization of cannabis. Tax revenues have significantly increased in states that have legalized cannabis. For instance, the monthly state marijuana tax and fee revenue that is posted in the Colorado state accounting system is shown in the Marijuana Tax Reports. The state’s retail marijuana sales tax, which accounts for 15% of retail marijuana sales, and the state’s retail marijuana excise tax, which accounts for 15% of wholesale sales and transfers of retail marijuana, all contribute to the state’s tax revenue. Fees for marijuana licenses and applications generate revenue. 8
Concerns about racial disparities in drug policing and shifting attitudes toward drug use and addiction have also had an impact on the legalization of cannabis. In many states, “cannabis policy is shifting from a criminal justice perspective to a public health and safety approach,” as noted in a report by the National Conference of State Legislatures. 9
The prohibition of cannabis has historically been used to oppress racial groups, according to the Drug War Statistics. 10 For instance, cannabis was portrayed as a dangerous and addictive drug in the early 1900s and was associated with Mexican immigrants and African American jazz musicians. Despite similar rates of drug use, Black Americans are significantly more likely than White Americans to be arrested for drug offenses. This stigma continues to this day. 11 The article also mentions that the failure of the War on Drugs played a role in the legalization of cannabis. The Conflict on Medications, which started during the 1970s, was planned to lessen drug use and medication-related wrongdoing through forceful policing. Notwithstanding, pundits contend that the Conflict on Medications has been insufficient and has prompted the mass imprisonment of peaceful medication guilty parties. 10
Several states have passed laws making cannabis legal for medical and/or recreational use to address these issues. Age restrictions and licensing requirements for dispensaries are 2 examples of the kinds of regulations that are typically included in these laws to lessen the negative effects of drug use. 12 However, the legalization of cannabis faces numerous obstacles, which may include worries about an increase in drug-related use and addiction. 13
Despite these difficulties, the trend toward the legitimization of marijuana will continue in the near future. 14 The legal landscape pertaining to cannabis is likely to become increasingly complex as public opinion continues to shift in favor of legalization and as more states adopt policies that are favorable to the use of cannabis. 7 In general, the legitimization of marijuana is a complicated issue, with different social and political variables driving its sanctioning at the state level. 15 It will be crucial to take into account the various dangers and benefits of cannabis, as well as the potential impact of cannabis policy on public health and safety, as the debate over its legalization progresses. 16
Active substances of marijuana
More than 500 chemicals have been identified in cannabis. However, the most extensively studied are cannabinoids, which are chemicals with 21 carbon atoms. 17 The cannabinoids found in marijuana are referred to as Phytocannabinoids, which are naturally occurring chemicals. 17 The active chemicals are Δ-9-tetrahydrocannabinol (THC), and cannabidiol (CBD). THC is the psychoactive ingredient, while CBD may also affect the brain and other organs in various ways. 2 , 17
Mechanism of action of marijuana
The human body has the endocannabinoid (eCB) system that plays a crucial role in the body by regulating functions such as sleep, eating, forgetting, relaxing, and protecting the body. The eCBs have a chemical structure that is similar to those of THC and CBD. 17 The common eCB is referred to as N -arachidonoylethanolamine or anandamide (AEA), which is located in the brain. 4 , 17 The second cannabinoid ligand found in the gastrointestinal tract is referred to as 2-arachidonoylglycerol (2-AG), which is located in the intestine. 4 After oral administration, THC and CBD will be hydrolyzed by the liver and then bind to the 2-AG receptors in the gastrointestinal tract. 17
The active Δ-9-tetrahydrocannabinol (THC) binds to the cannabinoid receptors in the brain cells, where it can interfere with various physical and mental functions. 4 , 17 The brain functions commonly affected by THC include memory, pleasure, balance, posture, and reaction time depending on the area of the brain. 5 These effects may be explained primarily by cannabinoids binding to the G- protein-coupled cannabinoid receptors CB1 and CB2. 17
The endocannabinoid system comprises the receptors CB1 and CB2, which respond to cannabinoids, the natural endogenous cannabinoids known as N -arachidonoylethanolamine (also called anandamide or AEA) and 2-arachidonoylglycerol (2-AG), as well as their respective enzymes for degradation, which are fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase. 18
CB1 receptors are mainly found on presynaptic peripheral and central nerve terminals, with lower expression in various other peripheral organs. In contrast, CB2 receptors are predominantly concentrated in peripheral tissues and immune cells, where they regulate the release of cytokines and cell migration. However, CB2 receptors are also present in the nervous system, albeit to a lesser extent. 19
CB1 receptors are primarily located in the cortex, hippocampus, spinal cord, cerebellum, basal ganglia, and hypothalamus. 17 The hippocampus and the cortex are regions of the brain connected to learning and memory. As a result, THC binding to CB1 receptors can impede an individual’s ability to create new memories or shift focus. 5 Similarly, THC and CBD may interfere with the normal functioning of the cerebellum and basal ganglia, which are essential for maintaining balance, reaction time, coordination, and posture. 5
Phyto-cannabinoids also bind with transient receptor potential (TPR) channels that are responsible for the transmission of ions, which may interfere with the transmission of neural signals. 17 THC, which has a stronger affinity than CBD, also attaches to monoamine transporters such as serotonin, norepinephrine, and dopamine 17 triggering the release of dopamine results in higher than normal levels. 17 Elevated dopamine levels produce 2 main effects. Firstly, it activates the reward system which created a euphoric effect. Secondly, since the system governs behavior such as sex and eating, THC makes marijuana to be addictive as other drugs.
Marijuana’s ability to interact with various endocrine systems forms the foundation for its potential use as a treatment for various conditions. Studies have shown that certain nervous system disorders such as migraines, Parkinson’s disease, multiple sclerosis, fibromyalgia, and irritable bowel syndrome may be caused by endocrine deficiencies due to genetic or physical factors. 17 Therefore, compounds like THC and CBD may be used to improve the management of these conditions as they have similar mechanisms to the cannabinoids found in the human body. However, the wide range of effects of marijuana suggests that it should only be used under medical supervision as it can have negative effects if abused.
Pharmacokinetic of cannabis
The way that THC, the psychoactive component of cannabis, is metabolized in the body depends on the method of consumption. 17 , 20 When taken orally, it is processed by the liver and converted into different metabolites, with the majority being eliminated in the feces and urine. 6
When consumed orally, THC is metabolized by the CYP450 enzyme system into 2 active metabolites: 11-OH-THC, which is psychoactive, and 11-COOH-THC, which is not. The majority of cannabis is eliminated from the body through feces as the 11-OH-THC metabolite (65%) and urine as the 11-COOH-THC metabolite (20%). 20 Research has shown that the amount of THC that can enter the bloodstream after being consumed orally is low, with a bioavailability of 4-12%. 17
Moreover, since THC is highly lipid-soluble, it is rapidly stored in fat tissues where it accumulates. 17 From these fat deposits, THC is slowly released back into the bloodstream. 17 On the other hand, if THC is inhaled its metabolites enter the bloodstream more quickly through the lung, and effects are felt within 6 to 10 minutes. 17 Furthermore, a study has shown that CYP2C9 polymorphisms can also lead to significant changes in THC bioavailability. 20 It has been found that CYP2C9 polymorphisms result in a reduction of CYP2C9 metabolic activity which leads to an increase in THC exposure 2- to 3-fold. This type of CYP2C9 polymorphism is highly prevalent up to 35% in white individuals compared with other racial groups. 20
Like THC, CBD, another chemical found in cannabis, enters the body and is metabolized into multiple metabolites, with the most prevalent being hydroxylated 7-COOH derivatives. 17 The pharmacokinetics of CBD compound is complex. When inhaled, its bioavailability is between 11% and 45%, but when taken orally it is around 6%. 20 Furthermore, like THC, CBD is highly lipid-soluble and distributes quickly into the brain, adipose tissues, and other organs. CBD can act as either an agonist or antagonist to their binding site. 17
Research indicates how THC and CBD interact with specific enzymes in the body especially cytochrome P450 isoenzymes, which can affect the metabolism of other drugs. 17 , 20 Some studies have shown that THC is a CYP1A2 inducer which leads to reduced drug concentration by increasing metabolism and consequently decreasing the drug effect. 17 , 20 On the other hand, CBD has been found to inhibit the activity of CYP3A4 and CYP2D6 enzymes, which can lead to an increase in drug concentration due to a reduction in metabolism, potentially leading to significant adverse effects. 17 , 20
The Effects of Marijuana on the Human Body
The effects on human cells.
THC and CBD also have a wide range of effects on human cells. The primary effects of THC on the cellular level include the formation of reactive oxygen species (ROS) formation which leads to alteration in lipid metabolism and triggers the release of inflammatory cytokines. 21
Inflammatory cytokines are classified into 2 categories: pro-inflammatory and anti-inflammatory. Pro-inflammatory cytokines cause inflammation and pain, while anti-inflammatory cytokines can decrease pain and reduce inflammation. It’s crucial to maintain a balance between the 2 types of cytokines. THC’s impact on this balance can lead to tissue damage, particularly in organs that are sensitive such as the lungs, liver, and kidneys. Furthermore, THC can cause oxidative stress by producing more reactive oxygen species (ROS) than the body’s antioxidant defense system can handle. 22 Oxidative stress results in the formation of free radicals, which are unstable radical molecules with unpaired electrons. Free radicals interact with biomolecules such as carbohydrates, proteins, and lipids, which can cause permanent changes.
Cannabinoids can also contribute to the development of atherogenesis in 2 main ways. Firstly, ROS, which is primarily caused by CB1 receptor agonists, can cause damage to endothelial cells. Additionally, CB2 receptor agonists can increase inflammation and decrease the expression of cell adhesion molecules. Furthermore, lipid metabolism may also be affected by the oxidation of low-density lipoprotein (ox-LDL), which can increase the expression of CB1 and CB2 receptors and enhance the production of endogenous cannabinoids. 23 As a result, it causes the accumulation of lipids in macrophages, which are specialized cells present in the liver and lungs that help eliminate harmful organisms. 23 , 24 Thus, the active compounds in cannabis can harm different types of cells, particularly in the lungs, liver, kidney, and heart.
Harmful effects of marijuana
The growing legalization and acceptance of marijuana have led to an increase in its use in America for both medicinal and recreational purposes. 25 In 2016 and 2017, more than 39 million Americans reported having used marijuana in the past year. 23 Delta-9-tetrahydrocannabinol (THC) is the most psychoactive in marijuana.
Various organs of the human body contain cannabinoid (CB1 and CB2) receptors, including the brain, peripheral nervous system, liver, skeletal muscles, and myocytes. 23 Due to the location of the cannabinoid receptors on multiple organs, marijuana can have various harmful effects, including interfering with learning ability, mental disorders, addiction, cardiovascular disorders, and certain types of cancers.
Cardiovascular disorders
Marijuana may also increase the risk of individuals developing cardiovascular disorders. Approximately 2 million Americans who have been diagnosed with cardiovascular disorders reported using marijuana. 26 It has been found that smoking marijuana is associated with cardiotoxicity, similar to the effects of smoking cigarettes. 27 Research has shown that smoking marijuana has similar cardiovascular risks as smoking cigarettes. Despite smoking fewer puffs, users inhale deeper and hold the smoke longer, raising the risk of cardiotoxicity. Additionally, marijuana increases the risk of patients diagnosed with cardiovascular disorders such as atherosclerotic or developing coronary artery disease. 26
A study previously revealed that cannabis consumption can raise heart rate and blood pressure, thereby increasing the demand for oxygen in the heart. Furthermore, prolonged use of marijuana may cause oxidative stress that leads to cellular damage, platelet activation, induction of an inflammatory response, and the formation of oxidized low-density lipoprotein cholesterol (ox-LDL). THC may also cause a release of catecholamines and beta-adrenergic stimulation, increasing the likelihood of arrhythmias. People who smoke marijuana have a 3.3 times greater risk of experiencing a cerebrovascular event. 21 Marijuana increases the risk of thrombosis and ischemia, which may contribute to the development of peripheral artery disease. 27 Thus, marijuana use can lead to multiple cardiovascular disorders, particularly in individuals who already have these conditions.
The relationship with cancer
Research has been conducted on the potential use of marijuana and specific compounds found in the plant, such as THC and CBD, to alleviate symptoms associated with cancer and cancer treatments, such as chemotherapy. Some evidence suggests that certain cannabinoids may be effective in managing these side effects. 14 It is important to note that marijuana can have adverse effects and potential complications. Choosing to avoid or postpone conventional medical treatment for cancer or relying solely on marijuana to manage the symptoms of cancer, can lead to serious health risks. 28
Studies on the compounds in marijuana, known as cannabinoids, have indicated that certain cannabinoids may be useful in managing symptoms of nausea and vomiting associated with chemotherapy, as well as in treating neuropathic pain. 28 Marijuana use introduces cannabinoids, including THC, into the body, but it also includes harmful substances such as toxins and carcinogens found in tobacco smoke that can harm the lungs and cardiovascular system. 29 , 30 While more research is needed to determine the effects of marijuana on lung and other respiratory cancers, limited evidence suggests a connection between marijuana smoking and testicular cancer. 14 , 31
The concentration levels of active compounds in marijuana vary depending on the form in which it is consumed, which may explain the different effects on different individuals. Further research is necessary to fully comprehend the effects of marijuana use on cancer. 32
Another research suggests that using marijuana can increase the risk of developing certain types of cancer. For instance, a study conducted in New York Hospital found that individuals who use marijuana have a 2.6 times higher risk of upper aerodigestive tract cancer. Similarly, there is significant evidence linking marijuana use to Human papillomavirus-16 (HPV-16) positive head and neck cancer. 33 Additionally, some studies have indicated that marijuana use can increase the risk of developing lung cancer by 8.2 times. However, it is worth noting that heavy cannabis use for over 10 joint years primarily puts adults aged 55 years and older at a higher risk of developing lung cancer. 34
Marijuana use for over 10 years has been associated with a 1.5 times higher risk of testicular cancer. Additionally, paternal marijuana use has been linked to an increased risk of myeloid leukemia in their children, and maternal marijuana use during the first trimester may increase the risk of neuroblastoma in the child by 4 times. 33
The effects of cannabis on cancer risk vary depending on the type of cancer, the affected organ, and the receptors that are stimulated. 35 This is due to changes in the representation of CB1 and CB2 receptors observed in various types of cancers. 35 , 36 For instance, in Hodgkin lymphoma and cellular hepatocarcinoma, the expression of CB1 receptors is increased. 35 Conversely, ovarian cancers are associated with increased severity when CB2 receptors are expressed. Additionally, there is a high correlation between the overexpression of CB2 receptors and human breast adenocarcinoma and glioma, both of which are linked to breast cancer and malignant brain tumors. 35
In addition, research has linked variations in CB1 and CB2 receptors to poor outcomes following surgery for stage IV colorectal cancer. 35 THC is the primary compound that has been linked to an increased risk of cancer development, and the specific tissue where CB1 and CB2 receptors are disrupted determines the likelihood of cellular abnormalities and changes in enzymes and neurotransmitters. 36 Dysregulation of the endocannabinoid system occurs when there is an overproduction or underproduction of CB1 and CB2 receptors, which can lead to several health problems, including cancer. 36 For instance, up-regulation of CB1 receptors without changes in the regulation of CB2 is associated with an increase in the risk of pancreatic cancer. Conversely, inhibiting CB1 receptors in the colon tissue may increase the risk of colon cancer.
Benefits of cannabis
Cannabis has been cultivated and used by people for recreational and medicinal purposes since ancient eras for the past of hundreds of years. 23 The main component with medicinal purposes is cannabidiol (CBD). CBD attaches to the endocannabinoid system, potentially influencing the nervous system by triggering the release of hormones and other natural compounds like dopamine. As a result, marijuana may be useful in the management of several disorders such as anxiety, psychiatric disorders, pain, and obesity. 23
Several studies have discovered the efficacy of cannabis in alleviating pain. For example, a study conducted by Wallace et al 37 found that moderate use of marijuana with a THC content of 4% was associated with pain relief. However, high doses (7%THC) of marijuana were found to increase pain 38 and low doses (1% THC) of marijuana did not have any impact on pain levels. 12 , 37 The main cannabis element that is used for pain management is Anandamide, which acts as an autocrine or paracrine messenger. 38 The chemical is broken down into arachidonic acid and ethanolamine. The chemical can modulate nociceptive signals that cause pain by activating local CB1 receptors. 38 Marijuana could also be used as an alternative to opioids to relieve pain, despite its risk of addiction, but it is not life-threatening as opioids.
Chronic pain is among the major health issues with a high burden on individuals and society in the US. About half of the physician visits are due to chronic pain, resulting in a total medical cost of approximately $600 billion annually. 38 Pain is often described as a subjective experience that involves sensory-physiological, cognitive-evaluative, and motivational effective components. In humans, there are 3 main types of pain: nociceptive, neuropathic, and central. 38 , 39 Nociceptive pain is caused by damage to the tissue and is considered a defensive mechanism. On the other hand, neuropathic pain is caused by damage to the sensory and spinal nerves. Central pain is caused by consistent damage to the central nervous system amplifying pain signals from the periphery. 40
Other drugs have been used to treat pain, including alcohol and nicotine. However, discontinued use of addictive substances increases pain sensitivity. Marijuana reduces pain by binding CB1 and CB2 receptors that are activated by tissue injury. 38 It also reduces pain by binding to transient receptor potential cation channel subfamily V member 1 (TRPV1) receptors which are mainly found in the nociceptive neurons of the peripheral nervous system. 39 TRPV1 receptors are also found in the central nervous system where they involve in the transmission and modulation of pain, as well as the integration of painful stimuli. 39
Targeting the endocannabinoid system to modulate pain is a promising way of managing pain, especially chronic pain. Anandamide (AEA) is also produced in injured cells, where it activates the local CB1 receptor, however, AEA is unable usually to activate all the CB1 receptors due to an enzyme called fatty acid amide hydrolase (FAAH) which converts it into Ethanol-amide or arachidonic acid (AA). Exogenous cannabinoids (cannabis) inhibit the FAAH enzyme, and this allows more CB1 receptors activation. 4 Additionally, 2-arachidonoyl glycerol (2-AG) is activated by CB1 receptors and acts as a massager for pain. 38 Since 2-AG is an endocannabinoid, it plays a central role in modulating pain. Therefore, cannabis may suppress pain in a similar way to endocannabinoids by activating CB1 and CB2 receptors. 38 - 40
Several research studies have demonstrated that cannabis is remarkably proficient in alleviating pain. For example, a randomized controlled trial found that there is a therapeutic window for using marijuana to reduce pain, particularly when it is smoked. 12 However, another research suggests that oral forms of marijuana can also reduce pain. While the onset of effects may be slower compared to smoking, the pain relief provided by oral consumption is typically longer-lasting. 41 Additionally, in a different randomized clinical trial, it was observed that the individuals in the intervention group had greater pain relief than those in the placebo group. 42 Cannabis is commonly used to manage chronic pain in individuals with multiple sclerosis and arthritis. 42
Recent advancements in treating pain among individuals with multiple sclerosis are using drugs that contain cannabis extracts, Sativex. 18 The main extracts that are used to treat pain that is not suppressed by traditional painkillers are cannabidiol and THC. 42 Moreover, Sativex (Nabiximols) is an oro-mucosal and is added in a ratio of 1:1 formulation of THC: CBD to increase the efficacy of suppressing pain. In a randomized blind control, 50% of patients reported experiencing pain reduction compared to only 30% in the placebo group. 42 Additionally, medical marijuana is used by approximately 9.33% of patients to manage joint pain associated with arthritis. 42 Medical cannabis can effectively alleviate pain from various chronic conditions, offering hope for many patients who experiencing chronic pain.
Cannabis can also be used to treat obesity, which is a risk factor for chronic illnesses such as diabetes and cardiovascular disorders. The chemical d-9-tetrahydrocannabivarin (d-9-THCV) found in marijuana can be used to treat obesity. d-9-THCV has anti-obesity effects by reducing food intake and increasing energy expenditure, leading to weight loss. 43 Additionally, Cannabis blocks CB1 receptors and activates CB2 receptors that can potentially treat disorders such as obesity and chronic liver disease, particularly if the conditions are associated with inflammation. 43
Cannabis may also be used to reduce social anxiety due to its neural, symptomatic, and electrodermal effects on fearful faces. Cannabis activates the limbic and paralimbic regions which reduce subjective anxiety and autonomic arousal. 43 Several human and animal studies have shown that CBD possesses anxiolytic properties that reduce social anxiety disorders. Additionally, research has indicated that CBD may be able to prevent acute psychosis. Marijuana is preferred over other antipsychotic drugs because it has relatively fewer side effects. 43
Cannabis can also be used to manage multiple sclerosis due to its anti-inflammatory and immunosuppressive properties that can assist individuals with hyperactive immune systems. 19 Moreover, cannabis has an apoptotic effect on immune cells, which may help patients with conditions such as rheumatoid arthritis, asthma, and other immune diseases. 39
The Effects of Marijuana on the Daily Lives of Individuals
The effects of marijuana use on education attainment.
Marijuana has various side effects on the brain that may interfere with learning ability and reduce lifetime achievement in young people. Studies have shown that marijuana use is linked to decreased learning ability which leads to lower educational attainment, particularly in individuals with high rates of marijuana use. 25 One possible explanation could be related to the adverse effect of marijuana on cognitive functions during acute intoxication and for days after use. 25 The use of marijuana can negatively impact academic performance by hindering a student’s natural abilities.
A review conducted by Silins et al, 44 indicated that marijuana use in adolescence can affect academic performance negatively if started early. The study found that people who started using cannabis before the age of 17 were less likely to complete secondary school or pursue higher education. Brook et al 45 in their longitudinal review found that marijuana use at an early age was connected to lower adult income and lower educational attainment.
Prolonged use of marijuana can also negatively affect memory and focus, which are essential for learning. The severity of these effects is heightened with regular use and early initiation. Furthermore, research suggests that the earlier someone starts using marijuana, the less education they are likely to attain. Those who begin using it at a younger age are less likely to achieve as much as those who start using it later in life.
Silins et al 44 found that adolescents who used marijuana frequently had a lower chance of graduating from high school than those who did not use it or used it sparingly. A study by Lynne-Landsman et al 46 found that teenagers who used marijuana frequently in adolescence had a lower chance of finishing high school or getting a degree from a college. Marijuana use can adversely affect work status as well as instructive results compared with the people who didn’t utilize marijuana or utilized it just once in a while.
Prolonged use of marijuana can have a detrimental impact on an individual’s overall life outcomes. Studies have shown a strong connection between marijuana use and factors such as low income, dependence on social services, criminal behavior, unemployment, and a lower sense of satisfaction with life. 25 The factors discussed are interconnected, where low income can lead to dissatisfaction with life and increase the likelihood of committing crimes and may be caused by unemployment which could be a result of criminal records. Additionally, low income can impede an individual’s ability to achieve their goals, such as buying a house or a car. Furthermore, marijuana use can negatively impact educational attainment, leading to unemployment or low wages, and ultimately, lower lifetime achievements. 25
Potential development of addiction
Marijuana is also an addictive substance and can lead to various social, economic, and physical issues. The addiction properties are mainly attributed to THC, which acts as a partial agonist for CB1, CB2, and peroxisome proliferator-activated receptors. 47 As a result, smoking marijuana can cause feelings of euphoria, easy laughter, talkativeness, and heightened sensitivity to external stimuli, which can make people willing and more likely to use the drug repeatedly. The level of addiction is determined by several factors, including vulnerability to mental illness, personality traits, and the content of THC. 48
The amount of THC has significantly increased from 8.5% in 1999 to 20% in 2004 through crossbreeding of hemp plants that contain high THC content. 48 Cannabis addiction shares similarities with other types of addiction, as it is a chronic condition characterized by repeated use, abstinence, and relapse. Additionally, individuals may experience withdrawal symptoms when they stop using marijuana.
Marijuana may have rewarding or aversive effects on the brain by interacting with CB1 and CB2 receptors in the ventral tegmental area (VTA) in the brain. 49 The rewarding effects of cannabis are caused by the activation of CB1 receptors on VTA GABAergic neurons, leading to an increase in dopamine release in the nucleus accumbens (NAc), resulting in feelings of euphoria. 50 However, when cannabis binds to CB1 receptors in the brain’s VTA and blocks the release of the neurotransmitter glutamate from glutamatergic neurons, it results in a decrease in dopamine activity in the reward center, leading to aversion and negative effects. 51
Mental health
The frequent use of marijuana is often linked to anxiety, a condition characterized by excessive fear. Marijuana’s impact on the brain can be particularly harmful to adolescents, whose brains are still developing, potentially altering the structure and function of various regions of the brain, such as the cerebellum, temporal, and frontal cortex, depending on the amount of marijuana used. 33 Moreover, cannabis may affect the amygdala located in the limbic system which may limit the ability of people to process emotions, which could affect the mood of the user. Cannabis may impact the limbic system, specifically the amygdala, which can affect a person’s ability to process emotions and affect their mood. It may also negatively impact the hippocampus and ventromedial prefrontal cortex, which can affect the brain’s ability to learn and remember. Long-term use may also lead to depression and psychoses, especially in those with a genetic vulnerability or preexisting mental illnesses such as schizophrenia. 23 Previous research suggests that starting to use marijuana at an early age can worsen the progression of mental disorders like schizophrenia, potentially causing the onset of a first psychotic episode 2 to 6 years earlier. 25
Marijuana use, especially in high doses and on a regular basis, can lead to disorientation as well as occasionally unpleasant thoughts or feelings of anxiety and paranoia, according to the Centers for Disease Control and Prevention (CDC). 13 People who use marijuana are more likely to develop both short-term psychosis (such as hallucinations and paranoia) and long-term mental disorders, such as schizophrenia. 52 The link between marijuana use and schizophrenia is stronger in people who start Pot use and has additionally been connected to despondency; social phobia; thoughts of suicide, attempts at suicide, and ultimately suicide. 14
A Systematic Review examined the use of cannabinoids to treat PTSD, anxiety disorders, and mood disorders. The authors indicated that cannabinoids may be effective in treating these conditions, but they suggested more research is needed to figure out the best cannabinoid dosages and formulations for different patient populations. In addition, the authors point out that there are risks associated with using cannabinoids to treat mental health conditions, such as the possibility of compulsion and adverse effects. The article emphasizes the necessity of continuing research in this area to better comprehend the likely benefits and risks of using cannabinoids in emotional wellness treatment. 53
Social impacts of marijuana
Marijuana use can differently affect school, work, and public activity, both positively and negatively. The Public Organization on Chronic drug use states that marijuana use can impede mental capacities, such as memory, consideration, and learning. According to NIDA (2020), this can negatively impact academic achievement and performance, resulting in lower grades and decreased motivation to succeed in school. 54
Marijuana use can have an impact on a person’s work performance as well as their academic performance. Marijuana use was linked to lower job performance and higher absenteeism, according to a study that was published in the Journal of Addictive Diseases . 55 As a result, there may be fewer job opportunities, lower income, and negative consequences. In addition, marijuana use can slow down one’s reaction time and motor skills, which can be dangerous in certain workplaces, like those where one must drive or operate heavy machinery. 54
Social life can also be impacted by marijuana use. While certain individuals might find that utilizing marijuana upgrades their social encounters by decreasing social stress and increasing feelings of relaxation, it can lead to unfavorable results. Marijuana use can prompt social withdrawal, diminished relational abilities, and diminished inspiration to participate in friendly exercises. 54
In addition, excessive marijuana use can result in addiction, which can have negative effects on every facet of life. The National Institute on Drug Abuse (NIDA) estimates that approximately 1 in 10 marijuana users will develop an addiction to the drug, and this percentage rises to 1 in 6 for adolescents who begin using marijuana. 54
It is essential to keep in mind that a variety of factors, including frequency and quantity of use, age at onset, and individual differences in susceptibility to the effects of the drug, can have an impact on how marijuana use affects school, work, and social life. Additionally, if marijuana use is stopped, some of the negative effects, such as impaired cognitive abilities, may be reversed. 54
Marijuana is a substance that is used for both recreational and medical purposes in large quantities, it is still one of the most widely used drugs in the United States and around the world. Marijuana has complicated pharmacokinetics that can have a variety of effects on cells, including the production of reactive oxygen species, changes in the formation of lipids, and the release of inflammatory cytokines. To better comprehend the pharmacological effects of marijuana on human health, additional research is required.
Even though cannabis has been shown to have several health benefits that could help treat and manage conditions like pain, obesity, anxiety, and multiple sclerosis, it is worth mentioning that it also has the potential to cause adverse effects. Marijuana use may still be linked to an increased risk of addiction, mental health disorders, certain types of cancer, impaired learning, and lower lifetime achievement despite having fewer side effects than prescription drugs like antipsychotics and opioids. As a result, when weighing the potential advantages and disadvantages of marijuana use, careful consideration is required.
While marijuana use can improve social interactions, it can also have a negative impact on social, academic, and professional functioning. The utilization of marijuana can hurt relational connections, reduce work environment efficiency, and weaken mental capacities. Public opinion, potential tax revenue, concerns about racial disparities in drug policing, and shifting attitudes toward drug use and addiction all have an impact on the contentious issue of legalizing cannabis in the United States. Concerns about an increase in drug-related addiction persist despite the fact that several states have legalized cannabis for medical and/or recreational use. The legal framework surrounding cannabis is anticipated to become increasingly complex as public opinion shifts toward legalization.
One limitation of the review article is that it does not explore the ideas and thoughts of individuals regarding their perceptions of the meaning, benefits, harms, or needs associated with their cannabis use. While the article may provide valuable knowledge and analysis based on available research and data, it does not dive into the subjective experiences and perspectives of the individuals themselves.
Author Contributions: The author confirms responsibility for the following: study conception and design, data collection, analysis and interpretation of results, and manuscript preparation.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
- 1. Ben Lesser NKARD. The History and Use of Marijuana in The Society. 2021. Accessed January 21, 2023. https://dualdiagnosis.org/marijana-treatment/reefer-madness-look-evolution-marijuana-society/
- 2. Zou S, Kumar U. Molecular sciences cannabinoid receptors and the endocannabinoid system: signaling and function in the central nervous system. Int J Mol Sci. 2018;19:833. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Narconon International. History of Marijuana. 2023. Accessed January 21, 2023. https://www.narconon.org/drug-information/marijuana-history.html
- 4. Bridgeman MB, Abazia DT. Medicinal cannabis: history, pharmacology, and implications for the acute care setting. P T. 2017;42:180-188. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. National Institute on Drug Abuse. How does marijuana produce its effects? NIDA. 2021. Accessed January 21, 2023. https://nida.nih.gov/publications/research-reports/marijuana/how-does-marijuana-produce-its-effects
- 6. Sidebari L. CRS Legal Sidebar Prepared for Members and Committees of Congress Recent Developments in Marijuana Law. 2022. Accessed January 21, 2023. https://crsreports.congress.gov
- 7. Daniller A. Two-thirds of Americans support marijuana legalization. Pew Research Center. 2023. Accessed April 28, 2023. https://www.pewresearch.org/short-reads/2019/11/14/americans-support-marijuana-legalization/
- 8. Marijuana Tax Reports. State of Colorado. 2023. Accessed April 28, 2023. https://cdor.colorado.gov/data-and-reports/marijuana-data/marijuana-tax-reports
- 9. Hartman M. The war on Marijuana. National Conference of State Legislatures. 2022. Accessed April 28, 2023. https://www.ncsl.org/civil-and-criminal-justice/cannabis-overview [ Google Scholar ]
- 10. Drug War Statistics. Drug Policy Alliance. 2022. Accessed April 28, 2023. https://drugpolicy.org/issues/drug-war-statistics
- 11. American Civil Liberties Union. Report: The war on Marijuana in Black and White. American Civil Liberties Union. 2023. Accessed April 28, 2023. https://www.aclu.org/report/report-war-marijuana-black-and-white?redirect=report/war-marijuana-black-and-white [ Google Scholar ]
- 12. Sacco LN. The Marijuana Policy Gap and the Path Forward. 2017. Accessed April 28, 2023. https://www.crs.gov
- 13. Marijuana and Public Health. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. 2020. Accessed April 28, 2023. https://www.cdc.gov/marijuana/health-effects/mental-health.html
- 14. National Academies of Sciences and Medicine E. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press; 2017. [ PubMed ] [ Google Scholar ]
- 15. Health Affairs. Cannabis legalization in the US: population health impacts. health-affairs-brief-cannabis-public-health-mauri. 2021. Accessed April 28, 2023. https://www.healthaffairs.org/do/10.1377/hpb20210701.500845/
- 16. Volkow N. Cannabis (Marijuana) Research Report. 2020. Accessed April 28, 2023. https://nida.nih.gov/download/1380/cannabis-marijuana-research-report.pdf?v=7fc7d24c3dc120a03cf26348876bc1e4 [ Google Scholar ]
- 17. Chayasirisobhon S. Mechanisms of action and pharmacokinetics of Cannabis. Perm J. 2020;25:1-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Serrano A, Parsons LH. Endocannabinoid influence in drug reinforcement, dependence and addiction-related behaviors. Pharmacol Ther. 2011;132:215-241. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. De Petrocellis L, Di Marzo V. An introduction to the endocannabinoid system: from the early to the latest concepts. Best Pract Res Clin Endocrinol Metab. 2009; 23:1-15. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Brown JD. Potential adverse drug events with tetrahydrocannabinol (THC) due to drug–drug interactions. J Clin Med. 2020;9:4. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Ravi D, Ghasemiesfe M, Korenstein D, Cascino T, Keyhani S. Associations between marijuana use and cardiovascular risk factors and outcomes a systematic review. Ann Intern Med. 2018;168:187-194. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Raja A, Ahmadi S, de Costa F, Li N, Kerman K. Attenuation of oxidative stress by cannabinoids and cannabis extracts in differentiated neuronal cells. Pharmaceuticals. 2020;13:1-16. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. DeFilippis EM, Bajaj NS, Singh A, et al. Marijuana use in patients with cardiovascular disease: JACC review topic of the week. J Am Coll Cardiol. 2020;75: 320-332. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Macrophages. British Society for Immunology. May21, 2021. Accessed March 14, 2023. https://www.immunology.org/public-information/bitesized-immunology/cells/macrophages
- 25. Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219-2227. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Panlilio L V., Goldberg SR, Justinova Z. Cannabinoid abuse and addiction: clinical and preclinical findings. Clin Pharmacol Ther. 2015;97:616-627. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Lafaye G, Karila L, Blecha L, Cannabis BA. Cannabinoids, and health. Dialogues Clin Neurosci. 2017;19:309-316. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Noori A, Miroshnychenko A, Shergill Y, et al. Opioid-sparing effects of medical cannabis or cannabinoids for chronic pain: a systematic review and meta-analysis of randomised and observational studies. BMJ Open. 2021;11:e047717. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Lushniak BD, Samet JM, Pechacek TF, et al. The Health consequences of smoking—50 years of progress : a report of the Surgeon General. 2014. Accessed January 18, 2023. https://stacks.cdc.gov/view/cdc/21569 [ Google Scholar ]
- 30. Moir D, Rickert WS, Levasseur G, et al. A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem Res Toxicol. 2008;21:494-502. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Gurney J, Shaw C, Stanley J, Signal V, Sarfati D. Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis. BMC Cancer. 2015;15:1-10. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Centers for Disease Control and Prevention. Cancer. October19, 2020. Accessed January 18, 2023. https://www.cdc.gov/marijuana/health-effects/cancer.html
- 33. Huang YHJ, Zhang ZF, Tashkin DP, Feng B, Straif K, Hashibe M. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Prev Biomark. 2015;24:15-31. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Aldington S, Harwood M, Cox B, et al. Cannabis use and risk of lung cancer: a case–control study. Eur Respir J. 2008;31:280-286. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Pellati F, Borgonetti V, Brighenti V, Biagi M, Benvenuti S, Corsi L. Cannabis sativa L. And nonpsychoactive cannabinoids: their chemistry and role against oxidative stress, inflammation, and cancer. Biomed Res Int. 2018; 2018:1691428. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Tutino V, Caruso MG, De Nunzio V, et al. Down-regulation of cannabinoid type 1 (CB1) receptor and its downstream signaling pathways in metastatic colorectal cancer. Cancers (Basel). 2019;11:708. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Wallace MS, Marcotte TD, Umlauf A, Gouaux B, Atkinson JH. Efficacy of inhaled cannabis on painful diabetic neuropathy. J Pain. 2015;16:616-627. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. Hill KP, Palastro MD, Johnson B, Ditre JW. Cannabis and pain: a clinical review. Cannabis Cannabinoid Res. 2017;2:96-104. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Muller C, Morales P, Reggio PH. Cannabinoid ligands targeting TRP channels. Front Mol Neurosci. 2019;11:487. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1-32. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Kondrad E. Sidebar: medical marijuana for chronic pain. N C Med J. 2013;74:210-211. [ PubMed ] [ Google Scholar ]
- 42. Blake DR, Robson P, Ho M, Jubb RW, McCabe S. Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology. 2006;45: 50-52. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Cannabis AZ. A complex plant: different compounds and different effects on individuals. Ther Adv Psychopharmacol. 2012;2:241-254. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44. Silins E, Horwood LJ, Patton GC, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;1:286-293. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Brook JS, Zhang C, Brook DW. Developmental trajectories of marijuana use from adolescence to adulthood personal predictors. Arch Pediatr Adolesc Med. 2011;165:55-60. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Lynne-Landsman SD, Bradshaw CP, Ialongo NS. Testing a developmental cascade model of adolescent substance use trajectories and young adult adjustment. Dev Psychopathol. 2010;22:933-948. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Marijuana W. Displeases. National Institute on Drug Abuse (NIDA); 2021:15. [ Google Scholar ]
- 48. Cancilliere MK, Yusufov M, Weyandt L. Effects of Co-occurring marijuana use and anxiety on brain structure and functioning: a systematic review of adolescent studies. J Adolesc. 2018;65:177-188. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Han X, He Y, Bi GH, et al. CB1 receptor activation on VgluT2-expressing glutamatergic neurons underlies Δ9-tetrahydrocannabinol (Δ9-THC)-induced aversive effects in mice. Sci Rep. 2017;7:1-15. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Fattore L, Fadda P, Spano MS, Pistis M, Fratta W. Neurobiological mechanisms of cannabinoid addiction. Mol Cell Endocrinol. 2008;286:S97-S107. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. John WS, Martin TJ, Nader MA. Behavioral determinants of cannabinoid self-administration in old world monkeys. Neuropsychopharmacology. 2017;42: 1522-1530. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Volkow ND, Swanson JM, Evins AE, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry. 2016;73:292-297. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Stanciu CN, Brunette MF, Teja N, Budney AJ. Evidence for use of cannabinoids in mood disorders, anxiety disorders, and PTSD: a systematic review. Psychiatr Serv. 2021;72:429-436. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. U.S. Department of Health and Human Services National Institutes of Health. How does marijuana use affect school, work, and social life? U.S. Department of Health and Human Services National Institutes of Health. 2020. Accessed April 28, 2023. https://nida.nih.gov/publications/research-reports/marijuana/how-does-marijuana-use-affect-school-work-social-life [ Google Scholar ]
- 55. Frone MR. Prevalence and distribution of illicit drug use in the workforce and in the workplace: findings and implications from a US national survey. J Appl Psychol. 2006;91:856. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (528.5 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
Weed Research publishes topical and innovative papers on all aspects of weeds - weeds being defined as plants that adversely impact the economic, aesthetic, or environmental aspects of a system.. Our topics include weed biology and ecology, integrated weed management, herbicide resistance, invasive species, genetics and genomics, and novel weed control technology.
Journal of Cannabis Research is a broad scope open access journal sponsored by the Institute of Cannabis Research at Colorado State University-Pueblo (USA). ... Skip to main content. ... Marijuana use is increasingly common among patients with chronic non-cancer pain (CNCP) and long-term opioid therapy (LTOT). ... Source Normalized Impact per ...
Marijuana is the most commonly used illicit drug in the United States. More and more states legalized medical and recreational marijuana use. Adolescents and emerging adults are at high risk for marijuana use. This ecological study aims to examine historical trends in marijuana use among youth along with marijuana legalization. Data (n = 749,152) were from the 31-wave National Survey on Drug ...
This paper presents the up-to-date reported investigations and opens many reflections and further research perspectives. Keywords: Cannabis sativa L., ethnobotany, chemical composition, biological activities, medicine, in silico, molecular docking. 1. Introduction. Cannabis sativa L. is an herbaceous plant belonging to the Cannabaceae family ...
The Journal of Cannabis Research is the official publication of the Institute of Cannabis Research (ICR), which was established in June 2016 through an innovative partnership between Colorado State University Pueblo, the state of Colorado, and Pueblo County.. The ICR is the first US multi-disciplinary cannabis research center at a regional, comprehensive institution.
Here we review previous research on the acute and long-term effects of cannabis use on the brain and behavior, and find that the three-stage framework of addiction applies to CUD in a manner similar to other drugs of abuse, albeit with some slight differences. ... A 2016 systematic review of 105 papers assessing the acute and chronic effects of ...
The paper will review different aspects of marijuana in 4 main domains. A thorough discussion of marijuana's definition, history, mechanism of action, pharmacokinetics, and effects on human cells will be given in the first domain. The second domain will concentrate on marijuana's negative effects, while the third domain will look at ...
Cannabis is one of the most widely used substances globally, with nearly 2.5% of the world population reporting past year cannabis use. 1 Cannabis use rates are particularly high in North America. In the U.S., 45% of individuals reported ever using cannabis and 18% reported using at least once annually in 2019. 2,3 In Canada, approximately 21% of people reported cannabis use in the past year ...
Cannabis, or marijuana, has potential therapeutic and medicinal properties related to multiple compounds, particularly Δ-9-tetrahydrocannabinol and cannabidiol. Over the past 25 years, attitudes toward cannabis have evolved rapidly, with expanding legalization of medical and recreational use at the state level in the United States and recreational use nationally in Canada and Uruguay. As a ...
Significant support exists in the United States for legalization of marijuana/cannabis. As of 2021, 36 states and four territories approved the legalization of medical cannabis via medical marijuana laws (MMLs), and 15 states and District of Columbia (DC) have adopted recreational marijuana laws (RMLs).